Anxiety disorders
Highlights
Anxiety Disorders
Anxiety disorders include:
- Generalized anxiety disorder (GAD)
- Panic disorder
- Phobic disorders, such as agoraphobia and social phobia
- Obsessive-compulsive disorder (OCD)
- Post-traumatic stress disorder (PTSD)
- Separation anxiety disorder
Risk Factors
Risk factors for anxiety disorders depend in part on the specific disorder. General risk factors include:
- Gender. With the exception of obsessive-compulsive disorder (OCD), women have twice the risk for most anxiety disorders as men.
- Age. Phobias, OCD, and separation anxiety show up early in childhood, while social phobia and panic disorder are often diagnosed during the teen years.
- Traumatic Events. Traumatic events can trigger anxiety disorders, particularly post-traumatic stress disorder.
- Medical Conditions. Although causal relationships have not been established, certain medical conditions have been associated with increased risk of panic disorder. They include migraines, obstructive sleep apnea, mitral valve prolapse, irritable bowel syndrome, chronic fatigue syndrome, and premenstrual syndrome.
Treatment
The standard approach to treating most anxiety disorders is a combination of talk therapy, such as cognitive-behavioral therapy (CBT), and an antidepressant medication. Other types of medications (benzodiazepines, azapirones, beta blockers, or atypical antipsychotics) may also be prescribed. A healthy lifestyle that includes exercise, adequate rest, and good nutrition can also help to reduce the impact of anxiety.
Introduction
Fear and stress reactions are essential for human survival. They enable people to pursue important goals and to respond appropriately to danger. In a healthy individual, the stress response (fight or flight) is provoked by a genuine threat or challenge and is used as a spur for appropriate action.
An anxiety disorder, however, involves an excessive or inappropriate state of arousal characterized by feelings of apprehension, uncertainty, or fear. The word is derived from the Latin, angere, which means to choke or strangle. The anxiety response is often not triggered by an external threat or danger. Nevertheless it can still paralyze the individual into inaction or withdrawal. An anxiety disorder persists, while an appropriate response to a threat resolves, once the threat is removed.
Anxiety disorders are classified according to the severity and duration of their symptoms and specific behavioral characteristics. Types of anxiety disorders include:
- Generalized anxiety disorder (GAD)
- Panic disorder
- Phobias
- Obsessive-compulsive disorder (OCD)
- Post-traumatic stress disorder (PTSD)
- Separation anxiety disorder (which is almost always seen in children)
GAD and panic disorder are the most common. Anxiety disorders are usually caused by a combination of psychological, physical, and genetic factors, and treatment is, in general, very effective.
Generalized Anxiety Disorder
Generalized anxiety disorder (GAD) is the most common anxiety disorder. It affects about 5% of Americans over the course of their lifetimes. It is characterized by:
- A more-or-less constant state of worry and anxiety, which is out of proportion to the level of actual stress or threat in one's life.
- The anxiety occurs on most days during a period of more than 6 months despite the lack of an obvious or specific stressor. (It worsens with stress, however.)
- Patients with GAD may experience physical symptoms (such as gastrointestinal complaints) in addition to, or even in place of, mental worries.
- People with GAD tend to be unsure of themselves, overly perfectionist, and conforming.
Given these conditions, a diagnosis of GAD is confirmed if three or more of the following symptoms are present (only one for children) on most days for 6 months:
- Being on edge or very restless
- Feeling tired
- Having difficulty with concentration
- Being irritable
- Having muscle tension
- Experiencing disturbed sleep
Symptoms can cause significant distress and impair normal functioning. To be classified as GAD, they should not be due to a medical condition, another mood disorder, or psychosis. GAD rarely occurs by itself. It typically occurs along with another type of anxiety disorder, depression, or substance abuse.
Panic Disorder
Panic disorder is characterized by periodic attacks of anxiety or terror (panic attacks). Panic attacks usually last 15 - 30 minutes, although residual effects can persist much longer.
Panic attacks can occur in nearly every anxiety disorder, not just panic disorder. In other anxiety disorders, however, there is always a cue or specific trigger for the attack. A diagnosis of panic disorder is made under the following conditions:
- A person experiences at least two recurrent, unexpected panic attacks.
- For at least a month following the attacks, the person fears that another will occur.
Symptoms of a Panic Attack. During a panic attack a person feels intense fear or discomfort and experiences at least four or more of the following symptoms:
- Rapid heart beat
- Sweating
- Shakiness
- Shortness of breath
- A choking feeling or a feeling of being smothered
- Dizziness
- Nausea
- Feelings of unreality
- Numbness
- Either hot flashes or chills
- Chest pain
- A fear of dying
- A fear of going insane
Women may be more likely than men to experience shortness of breath, nausea, and feelings of being smothered. Men may be more likely than women to have sweating and abdominal pain. Panic attacks that include only one or two symptoms, such as dizziness and heart pounding, are known as limited-symptom attacks. These may be either residual symptoms after a major panic attack or precursors to full-blown attacks.
Frequency of Panic Attacks. Frequency of attacks can vary widely. Some people have frequent attacks (for example, every week) that occur for months; others may have clusters of daily attacks followed by weeks or months of remission.
Triggers of Panic Attacks. Panic attacks may occur spontaneously or in response to a particular situation. Recalling or re-experiencing even harmless circumstances that accompanied an earlier attack may trigger subsequent panic attacks.
Phobic Disorders
Phobias, manifested by overwhelming and irrational fears, are common. In most cases, people can avoid or at least endure phobic situations, but in some cases, as with agoraphobia, the anxiety associated with the feared object or situation can be incapacitating.
Agoraphobia. Agoraphobia is described as fear of being in public places or open areas. (The term comes from the Greek word agora, meaning outdoor marketplace.) In its severest form, agoraphobia is characterized by a paralyzing terror of being in places or situations from which the patient feels there is neither escape nor accessible help in case of an attack. Consequently, people with agoraphobia confine themselves to places in which they feel safe, usually at home. The patient with agoraphobia often makes complicated plans in order to avoid confronting feared situations and places.
Social Phobia. Social phobia, also known as social anxiety disorder, is the fear of being publicly scrutinized and humiliated and is manifested by extreme shyness and discomfort in social settings. This phobia often leads people to avoid social situations and is not due to a physical or mental problem (such as stuttering, acne, or personality disorders).
The associated symptoms vary in intensity, ranging from mild and tolerable anxiety to a full-blown panic attack. (Unlike a panic attack, however, social phobia is always directly related to a social situation.) Symptoms include sweating, shortness of breath, pounding heart, dry mouth, and tremor.
The disorder may be further categorized as generalized or specific social phobia:
- Generalized social phobia is the fear of being humiliated in front of other people during nearly all social situations. People with this subtype are the most socially impaired and also the most likely to seek treatment.
- Specific social phobia usually involves a phobic response to a specific event. Performance anxiety ("stage fright") is the most common specific social phobia and occurs when a person must perform in public. These patients usually feel comfortable in informal social situations.
Children with social anxiety develop symptoms in settings that include their peers, not just adults, and these symptoms may include tantrums, blushing, or not being able to speak to unfamiliar people. These children are often able to have normal social relationships with familiar people, however.
Specific Phobias. Specific phobias (formerly simple phobias) are an irrational fear of specific objects or situations. Specific phobias are very common. Most cases are mild and not significant enough to require treatment.
The most common specific phobias are fear of animals (usually spiders, snakes, or mice), flying (pterygophobia), heights (acrophobia), water, injections, public transportation, confined spaces (claustrophobia), dentists (odontiatophobia), storms, tunnels, and bridges.
When confronting the object or situation, the phobic person experiences panicky feelings, sweating, avoidance behavior, difficulty breathing, and a rapid heartbeat. Most phobic adults are aware of the irrationality of their fear, and many endure intense anxiety rather than disclose their disorder.
Obsessive-Compulsive Disorder
Obsessive-compulsive disorder (OCD) is a condition marked by unwanted intrusive and repeated thoughts (obsessions) and behaviors (compulsions):
- Obsessions are recurrent or persistent mental images, thoughts, or ideas. The obsessive thoughts or images can range from mundane worries about whether one has locked a door to bizarre and frightening fantasies of behaving violently toward a loved one.
- Compulsive behaviors are repetitive, rigid, and self-directed routines that are intended to prevent the manifestation of an associated obsession. Such compulsive acts might include repetitive checking for locked doors or unlit stove burners or calls to loved ones at frequent intervals to be sure they are safe. Some people are compelled to wash their hands every few minutes or to spend inordinate amounts of time cleaning their surroundings in order to subdue the fear of contagion.
A critical feature in this disorder is an overinflated sense of responsibility, in which the patient's thoughts center on possible dangers and an urgent need to do something about them. Over half of patients with OCD have obsessive thoughts without the ritualistic compulsive behavior. Although individuals recognize that the obsessive thoughts and ritualized behavior patterns are senseless and excessive, they cannot stop them in spite of strenuous efforts to ignore or suppress the thoughts or actions. OCD often accompanies depression or other anxiety disorders. Some patients find that their symptoms subside over time, while others experience a worsening of symptoms.
Symptoms in children may be mistaken for behavioral problems (taking too long to do homework because of perfectionism, refusing to perform a chore because of fear of germs). Children do not usually recognize that their obsessions or compulsions are excessive.
Associated Obsessive Disorders. Certain other disorders that may be part of, or strongly associated with, the OCD spectrum include:
- Body dysmorphic disorder (BDD). In BDD, people are obsessed with the belief that they are ugly, or part of their body is abnormally shaped.
- Hypochondriasis. People who are hypochondriacs have an excessive fear of having a serious disease.
- Anorexia nervosa. OCD frequently accompanies this eating disorder, where the compulsive behavior focuses on food restriction and thinness.
- Trichotillomania. People with trichotillomania continually pull their hair, leaving bald patches.
- Tourette syndrome. Symptoms of Tourette syndrome include jerky movements, tics, and uncontrollably uttering obscene words.
Obsessive-Compulsive Personality. OCD should not be confused with obsessive-compulsive personality, which defines certain character traits (being a perfectionist, excessively conscientious, morally rigid, or preoccupied with rules and order). These traits do not necessarily occur in people with obsessive-compulsive disorder.
Post-Traumatic Stress Disorder
Post-traumatic stress disorder (PTSD) is a severe, persistent emotional reaction to a traumatic event that severely impairs one’s life. It is classified as an anxiety disorder because of its symptoms. Not every traumatic event leads to PTSD, however. There are two criteria that must be present to qualify for a diagnosis of PTSD:
- The patient must have directly experienced, witnessed, or learned of a life-threatening or seriously injurious event.
- The patient's response is intense fear, helplessness, or horror. Children may behave with agitation or with disorganized behavior.
Triggering Events. PTSD is triggered by violent or traumatic events that are usually outside the normal range of human experience. War is a prime example. There is some evidence that events most likely to trigger PTSD are those that involve deliberate and destructive behavior (such as murder or rape) and those that are prolonged or physically challenging. Such events include, but are not limited to, experiencing or witnessing sexual assaults, accidents, military combat, natural disasters (such as earthquakes), or unexpected deaths of loved ones. PTSD may also occur in people who have serious illness and receive aggressive treatments or who have close family members or friends with such conditions.
Symptoms of PTSD. There are three basic sets of symptoms associated with PTSD. They may begin immediately after the event or can develop up to a year afterward:
- Re-experiencing. In such cases, patients persistently re-experience the trauma in at least one of the following ways: in recurrent images, thoughts, flashbacks, dreams, or feelings of distress at situations that remind them of the traumatic event. Children may engage in play, in which traumatic events are enacted repeatedly.
- Avoidance. Patients may avoid reminders of the event, such as thoughts, people, or any other factors that trigger recollection. They tend to have an emotional numbness, a sense of being in a daze or of losing contact with their own identity or even external reality. They may be unable to remember important aspects of the event.
- Increased Arousal. This includes symptoms of anxiety or heightened awareness of danger (sleeplessness, irritability, being easily startled, or becoming overly vigilant to unknown dangers).
To further qualify for a diagnosis of PTSD, patients must have at least one symptom in the re-experiencing category, three avoidance symptoms, and two arousal symptoms. Symptoms are chronic (3 months or more). Symptoms should also not be associated with alcohol, medications, or drugs and should not be intensifications of a pre-existing psychological disorder.
Acute Stress Disorder. In a syndrome called acute stress disorder, symptoms of PTSD occur within 2 days to 4 weeks after the traumatic event. Most people with acute stress disorder go on to develop PTSD.
Long-Term Outlook. The long-term impact of a traumatic event is uncertain. PTSD may cause physical changes in the brain, and in some cases the disorder can last a lifetime.
Separation Anxiety Disorder
Separation anxiety disorder almost always occurs in children. It is suspected in children who are excessively anxious about separation from important family members or from home. For a diagnosis of separation anxiety disorder, the child should also exhibit at least three of the following symptoms for at least 4 weeks:
- Extreme distress from either anticipating or actually being away from home or being separated from a parent or other loved one
- Extreme worry about losing or about possible harm befalling a loved one
- Intense worry about getting lost, being kidnapped, or otherwise separated from loved ones
- Frequent refusal to go to school or to sleep away from home
- Physical symptoms such as headache, stomach ache, or even vomiting, when faced with separation from loved ones
Separation anxiety often disappears as the child grows older, but if not addressed, it may lead to panic disorder, agoraphobia, or combinations of anxiety disorders.
Causes
An individual's genes, biochemistry, environment, personal history, and psychological profile can all contribute to the development of anxiety disorders. Most people with these disorders seem to have a biological vulnerability to stress, making them more susceptible to environmental stimuli than the rest of the population.
Biochemical Factors
Studies suggest that an imbalance of certain substances called neurotransmitters (chemical messengers in the brain) may contribute to anxiety disorders. The neurotransmitters targeted in anxiety disorders are gamma-aminobutyric acid (GABA), serotonin, dopamine, and epinephrine. Serotonin appears to be specifically important in feelings of well being, and deficiencies are highly related to anxiety and depression. Stress hormones such as cortisol also play a role.
Brain Structure Factors
Studies using imaging techniques, particularly magnetic resonance imaging (MRI), have helped to identify different areas of the brain associated with anxiety responses.
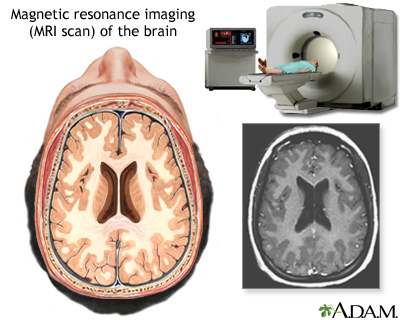
In particular, research has focused on changes in the amygdala, which is sometimes referred to as the "fear center." This part of the brain regulates fear, memory, and emotion and coordinates these resources with heart rate, blood pressure, and other physical responses to stressful events. Some evidence suggests that the amygdala in people with anxiety disorders is highly sensitive to new or unfamiliar situations and reacts with a high stress response.
Obsessive-compulsive disorder (OCD) is the anxiety disorder most strongly associated with specific brain dysfunction. For example, abnormalities in a specific pathway of nerves have been linked to OCD, attention deficit disorder, and Tourette syndrome. The symptoms of the three disorders are similar and they often occur together.
Several imaging studies have reported less volume in the hippocampus in people with post-traumatic stress disorder. This important region is related to emotion and memory storage.
Genetic Factors
Up to 50% of people with panic disorder and 40% of patients with generalized anxiety (GAD) have close relatives with the disorder.
Obsessive-compulsive disorder (OCD) is also strongly related to a family history of the disorder. Close relatives of people with OCD are up to 9 times more likely to develop OCD themselves. Researchers are making progress in identifying specific genetic factors that might contribute to an inherited risk. Of particular interest are genes that regulate specific neurotransmitters (brain chemical messengers), including serotonin and glutamate.
Risk Factors
Up to 25% of American adults experience intense anxiety sometime in their lives. The prevalence of true anxiety disorders is much lower, although they are still the most common psychiatric conditions in the United States and affect more than 20 million Americans.
General Risk Factors for Anxiety Disorders
Gender. With the exception of obsessive-compulsive disorder (OCD), women have twice the risk for most anxiety disorders as men. A number of factors may increase the reported risk in women, including cultural pressures to meet everyone else's needs except their own, and fewer self-restrictions on reporting anxiety to doctors.
Age. In general, phobias, OCD and separation anxiety show up early in childhood, while social phobia and panic disorder are often diagnosed during the teen years. Studies suggest that 3 - 5% of children and adolescents have some anxiety disorder. Children and adolescents who have an anxiety disorder are at risk of later developing other anxiety disorders, depression, and substance abuse.
Personality Factors. Children's personalities may indicate higher or lower risk for future anxiety disorders. For example, research suggests that extremely shy children and those likely to be the target of bullies are at higher risk for developing anxiety disorders later in life. Children who cannot tolerate uncertainty tend to be worriers, a major predictor of generalized anxiety. In fact, such traits may be biologically based and due to a hypersensitive amygdala -- the "fear center" in the brain.
Family History and Dynamics. Anxiety disorders tend to run in families. Genetic factors may play a role in some cases, but family dynamics and psychological influences are also often at work. Several studies show a strong correlation between a parent's fears and those of the offspring. Although an inherited trait may be present, some researchers believe that many children can "learn" fears and phobias, just by observing a parent or loved one's phobic or fearful reaction to an event.
Social Factors. Several studies have reported a significant increase in anxiety levels in children and college students in the past two decades compared to children in the 1950s. In several studies, anxiety was associated with a lack of social connections and a sense of a more threatening environment. It also appears that more socially alienated populations have higher levels of anxiety. For example, a study of Mexican adults living in California reported that native-born Mexican Americans were three times more likely to have anxiety disorders (and even more likely to be depressed) as those who had recently immigrated to the U.S. The longer the immigrants lived in the U.S., the greater their risk for psychiatric problems. Traditional Mexican cultural and social ties seemed to protect recently arrived immigrants from mental illness.
Traumatic Events. Traumatic events may trigger anxiety disorders, especially in individuals who are susceptible to them because of psychological, genetic, or biochemical factors. The clearest example is post-traumatic stress disorder. Specific traumatic events in childhood, particularly those that threaten family integrity, such as spousal or child abuse, can also lead to other anxiety and emotional disorders. Some types of specific phobias, for instance of spiders or snakes, may be triggered and perpetuated after a single traumatic exposure.
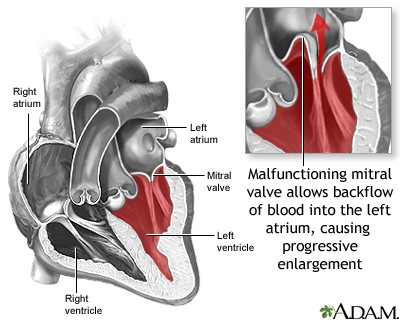
Medical Conditions. Although causal relationships have not been established, certain medical conditions have been associated with increased risk of panic disorder. They include migraines, obstructive sleep apnea, mitral valve prolapse, irritable bowel syndrome, chronic fatigue syndrome, and premenstrual syndrome.
Specific Risk Factors for Generalized Anxiety (GAD)
GAD affects about 1 - 5% of Americans in the course of their lives and is more common in women than in men. It is the most common anxiety disorder among the elderly. GAD usually begins in childhood and often becomes a chronic ailment, particularly when left untreated. Depression commonly accompanies this anxiety disorder, and depression in adolescence may be a strong predictor of GAD in adulthood.
Specific Risk Factors for Panic Disorder
Panic disorder usually first occurs either in late adolescence or when adults are in their mid-30s. Women have about twice the risk for panic disorder as men. Panic attacks are very common after menopause. The effects of pregnancy on panic disorder appear to be mixed. It seems to improve the condition in some women and worsen it in others.
Specific Risk Factors for Obsessive-Compulsive Disorder (OCD)
Obsessive-compulsive disorder occurs equally in men and women, and it affects about 2 - 3% of people over a lifespan. Most cases of OCD first develop in childhood or adolescence, although the disorder can occur throughout the lifespan.
Specific Risk Factors for Social Phobias
Social anxiety disorder is estimated to be the third most common psychiatric disorder in the U.S. Studies have reported a prevalence of 7 - 12% in Western nations.
Social anxiety disorder usually develops during the early teenage years. Women are more likely to develop social anxiety disorder than men, although equal numbers of men and women seek treatment for it. Most people seeking treatment have had symptoms for at least 10 years.
Specific Risk Factors for Post-Traumatic Stress Disorder
Traumatic events are the main risk factor for PTSD, but some people can go through such events and not experience PTSD. Studies estimate that 6 - 30% or more of trauma survivors develop PTSD, with children and young people being among those at the high end of the range. Women have the twice the risk of PTSD as men.
Researchers are trying to determine factors that might increase vulnerability to catastrophic events and put people at risk for develop PTSD. Some studies report the following may be risk factors:
- Pre-existing emotional disorder. People are at higher risk for PTSD if they have a history of an emotional disorder, particularly depression, before a traumatic event.
- Drug or alcohol abuse
- A family history of anxiety
- A history of physical or sexual abuse, neglect, or abuse within the family
- An early separation from parents
- Lack of social support and poverty
- Sleep disorders. Insomnia and excessive daytime sleepiness even within a month after a traumatic event are important predictors for the development of PTSD. One specific sleep disorder -- sleep apnea -- may even intensify symptoms of PTSD, including sleeplessness and nightmares. Sleep apnea occurs when tissues in the upper throat (or airway) collapse at intervals during sleep, thereby blocking the passage of air. Sleep apnea has also been associated with a risk for panic disorder. [For more information, see In-Depth Report #65: Sleep apnea.]
Complications
All types of anxiety disorders can be very debilitating and seriously affect a person’s quality of life.
Association with Depression and Bipolar Disorders
Depression. Depression is very common in people with an anxiety disorder, and it is sometimes difficult to distinguish between the two conditions. Both can have symptoms of anxiety, agitation, insomnia, and poor concentration. The combination of depression and anxiety is a major risk factor for both substance abuse and suicide.
Bipolar Disorder. Symptoms of panic disorder are very common in people with bipolar disorder. Furthermore, anxiety worsens bipolar disorder.
Increased Risk for Suicide
Panic disorder is associated with a risk for suicidal thoughts. Social phobias and OCD also increase the risk of suicide. If a person has an anxiety disorder and a mood disorders (such as depression), the risk for suicide is even higher. [For more information on suicide risks and prevention, see In-Depth Report #8: Depression.]
Increased Risk for Substance Abuse
Severely depressed or anxious people are at high risk for alcoholism, smoking, and other forms of addiction. Sometimes people with anxiety disorders may turn to these substances as a form of self-medication.
Effects on Work, School, and Relationships
Anxiety disorders can have negative effects on work and relationships.
Physical Effects of Anxiety Disorders in Adults
Anxiety disorders are associated with many different physical illnesses.
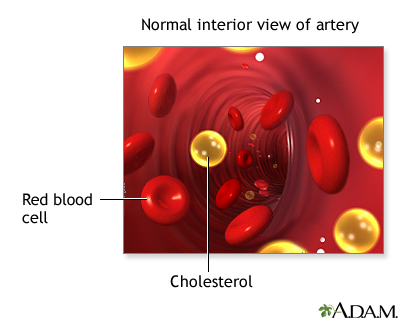
Heart Disease. Anxiety has been associated with several heart risk factors, including unhealthy cholesterol levels, thicker blood vessels, and high blood pressure. Both anxiety and depression have been associated with a poorer response to treatment in heart patients, including a worse outcome after heart surgery. The role of anxiety disorders in triggering serious cardiac events remains unclear.
Gastrointestinal Disorders. Anxiety frequently accompanies gastrointestinal conditions, particularly irritable bowel syndrome.
Headache. Both tension and migraine headaches are associated with anxiety disorders.
Respiratory Problems. Studies report an association between anxiety in patients with obstructive lung conditions (such as asthma, emphysema, and chronic bronchitis) and more frequent relapses.
Obesity. Anxiety disorders may lead to obesity, and the reverse may also be true.
Allergic Conditions. Anxiety disorders are associated with numerous allergic conditions including hay fever, eczema, hives, food allergies, and conjunctivitis.
Other Conditions. People with obsessive-compulsive disorders can experience skin problems from excessive washing, injuries from repetitive physical acts, and hair loss from repeated hair pulling (behavior known as trichotillomania).
Physical Effects of Anxiety Disorders in Children
Children with anxiety disorders often suffer from recurrent stomach aches. Anxiety has been associated with a higher risk for sleep disorders in children, such as frequent nightmares, restless legs syndrome, and bruxism (the grinding and gnashing of the teeth during sleep).
Diagnosis
Because anxiety accompanies so many medical conditions, some serious, it is extremely important for the doctor to uncover any medical problems or medications that might underlie or be masked by an anxiety attack. The doctor will perform a physical examination and ask about the patient’s medical and personal history.
The patient should describe any occurrence of anxiety disorders or depression in the family and mention any other contributing factors, such as excessive caffeine use, recent life changes, or stressful events.
It is very important to be honest with your doctor about all conditions, including excessive drinking, substance abuse, or other psychological or mood states that might contribute to, or result from, the anxiety disorder.
Diagnosing children with an anxiety disorder can be very difficult, since anxiety often results in disruptive behaviors that overlap with attention-deficit hyperactivity disorder or oppositional disorder. Other conditions with symptoms similar to anxiety disorders include pervasive developmental disorders such as Asperger syndrome, learning disabilities, bipolar disorder, and depression. Many children have anxiety disorder and a co-occurring condition, which should be treated along with anxiety.
Other Conditions with Similar Symptoms
People with anxiety disorders are more likely to see a family doctor before a mental health specialist, since their symptoms are often physical. Symptoms can include muscle tension, trembling, twitching, aching, soreness, cold and clammy hands, dry mouth, sweating, nausea or diarrhea, or urinary frequency. Anxiety attacks can mimic or accompany nearly every acute disorder of the heart or lungs, including heart attacks and angina (chest pain). In fact, nearly all individuals with panic disorders are convinced that their symptoms are physical and possibly life-threatening.
Heart Problems. Some patients who enter the emergency room with chest pain, and who have a low-to-moderate risk for a heart attack, are actually suffering from panic attacks. It is often difficult even for specialists to distinguish between heart conditions and a panic attack:
- Women who are having an actual heart attack or acute heart problem are much more likely to be misdiagnosed as having an anxiety attack than are men with similar symptoms.
- Mitral valve prolapse, a common and usually mild heart problem, may have symptoms that are nearly identical to those of panic disorder. The two conditions, in fact, frequently occur together.
- People with a heart-rhythm disturbance called paroxysmal supraventricular tachycardia have many of the same symptoms as those with panic attacks.
Asthma. Asthma attacks and panic attacks have similar symptoms and can also coexist.
Hyperthyroidism. Hyperthyroidism (overactive thyroid gland) can cause many of the same symptoms of generalized anxiety disorder.
Other Medical Conditions. Anxiety-like symptoms are seen in many other medical problems, including hypoglycemia (low blood sugar), recurrent pulmonary emboli, and adrenal-gland tumors. Women can also experience intense anxiety attacks with hot flashes during menopause.
Medication Side Effects. Many drugs, including some for high blood pressure, diabetes, and thyroid disorders, can produce symptoms of anxiety. Withdrawal from certain drugs, often those used to treat sleep disorders or anxiety, can also precipitate anxiety reactions.
Substance Abuse. People with anxiety disorders often drink alcohol or abuse drugs in order to conceal or eliminate symptoms, but substance abuse and dependency can also cause anxiety. In addition, withdrawal from alcohol can produce physiologic symptoms similar to panic attacks. Clinicians often have difficulty determining whether alcoholism or anxiety is the primary disorder. Overuse of caffeine or abuse of amphetamines can cause symptoms resembling a panic attack.
Screening Tests
Clinicians use various screening tests to determine the causes, type, severity, and frequency of anxiety. Such tests include the Hamilton Anxiety Rating Scale, the Beck Anxiety Inventory, the Social Phobia Inventory, the Penn State Worry Questionnaire, the Generalized Anxiety Disorder Scale, and the Yale-Brown Obsessive Compulsive Scale.
Treatment
The standard approach to treating most anxiety disorders is a combination of talk therapy, such as cognitive-behavioral therapy (CBT), and an antidepressant medication. A selective serotonin reuptake inhibitor (SSRI) is typically the first choice, with the serotonin-norepinephrine reuptake inhibitor (SNRI) venlafaxine (Effexor, generic) being an alternative. If patients do not respond to these drugs, tricyclic antidepressants may be helpful. Benzodiazepines may be recommended for patients who are not helped by antidepressants or who need help rapidly (antidepressants take several weeks to be effective). A healthy lifestyle that includes exercise, adequate rest, and good nutrition can also help to reduce the impact of anxiety.
Treatment Options for Specific Anxiety Disorders | ||
Anxiety Disorder | Medications | Cognitive-Behavioral Therapy (CBT) and other Non-Drug Therapies |
Generalized Anxiety Disorder | Antidepressants, benzodiazepines, and buspirone are helpful but have varying side effects. Investigational drugs include pregabalin and other anticonvulsants. | Cognitive-behavioral therapy or anxiety management therapy. Anxiety management therapy involves education, relaxation training, and exposure to anxiety-provoking stimuli but does not include cognitive restructuring. |
Panic Attacks | SSRIs are treatment of choice. If patients do not respond to SSRIs, short-term treatment with a benzodiazepine may be used, or patients may switch to another type of antidepressant such as venlafaxine or tricyclics. | Cognitive-behavioral therapy, provided in 12 - 16 sessions over 3 - 4 months, focuses on recreating fear symptoms and helping patients change their response to them. |
Social Anxiety Disorder | SSRIs or venlafaxine are first-line drug treatments. Benzodiazepines may help patients who do not respond to these antidepressants. Anticonvulsants such as gabapentin (Neurontin) and pregabalin (Lyrica) are being investigated. | Cognitive-behavioral therapy can help improve symptoms after 6 - 12 weeks. |
Obsessive-Compulsive Disorder | SSRIs are the first choice for adults. Clomipramine (a tricyclic antidepressant) is an alternative for adult patients who do not respond to SSRIs. For children, SSRIs do not seem to work as well for OCD as for other types of anxiety disorders. | Cognitive-behavioral therapy is the first treatment choice for children. For adults, either CBT or drug therapy may be offered as initial treatment. CBT techniques focus on exposure and response prevention (ERP). |
Post-Traumatic Stress Disorder | Antidepressants, particularly SSRIs (sertraline and paroxetine approved for PTSD). An atypical antipsychotic may be added to an antidepressant for patients who do not respond to a SSRI alone. | Trauma-focused psychological treatments include exposure therapy, trauma-focused cognitive therapy, and eye movement desensitization and reprocessing. |
Note: For anxiety disorders in adults, the most effective treatments are usually combinations of drugs and CBT techniques. For children, CBT is usually the first treatment. | ||
Medications
Selective serotonin-reuptake inhibitors (SSRIs), or the serotonin-norepinephrine reuptake inhibitor (SNRI) venlafaxine (Effexor, generic), are the primary first-line treatment for anxiety disorders. For patients who are not helped by these drugs or who need help rapidly, benzodiazepines may be prescribed, either alone or in combination with an antidepressant. Other types of antidepressants, including tricyclic antidepressants, may also be used to treat patients with severe or chronic forms of anxiety disorders.
Drug therapies for anxiety disorders work best in combination with cognitive behavioral therapy or some other form of psychotherapy.
Antidepressants
Selective Serotonin Reuptake Inhibitors (SSRIs). SSRIs include fluoxetine (Prozac, generic), sertraline (Zoloft, generic), paroxetine (Paxil, generic), fluvoxamine (Luvox, generic), citalopram (Celexa, generic), and escitalopram (Lexapro).
SSRIs can cause agitation, nausea, and diarrhea. Sexual dysfunction, including lowered sex drive, is a common side effect of many antidepressants as is weight gain. Elderly people taking these drugs should take the lowest effective dose possible, and those with heart problems should be monitored closely.
Antidepressants may raise the risk for suicidality (suicidal thoughts and behavior) in young people, particularly those ages 18 - 24. Both adults and children who are treated with SSRIs should be carefully monitored for any worsening of depressive symptoms or changes in behavior. This is especially important during the first few months of antidepressant treatment.
Paroxetine has been linked to heart-related birth defects when used during the first trimester of pregnancy. It should not be taken by women who are pregnant or planning on becoming pregnant. Other SSRIs are generally considered safe for use during pregnancy and breastfeeding. Still, women who are pregnant or who are considering becoming pregnant should discuss the potential risks of these drugs with their doctors.
Serotonin-norepinephrine reuptake inhibitors (SNRIs). SNRIs are known as dual action inhibitors because they work on two neurotransmitters -- norepinephrine and serotonin. Venlafaxine (Effexor. generic) is an SNRI that is approved for treatment of generalized anxiety disorder, social anxiety disorder, and panic disorder, Duloxetine (Cymbalta) is approved for treatment of generalized anxiety disorder. Both of these SNRIs are approved for adults but not for children
As with many SSRIs, venlafaxine impairs sexual function. Venlafaxine can increase blood pressure and heart rate and should be used with caution in patients with high blood pressure or heart disease. Some patients report severe withdrawal symptoms, including dizziness and nausea. This drug has a serious risk for overdose. Venlafaxine should not be taken during the last trimester of pregnancy because the drug can cause complications in newborn infants. A chemically related drug, desvelafaxine (Pristiq), is approved for treatment of depression has not yet been approved for treatment of anxiety.
Duloxetine's side effects are generally mild and include dry mouth, nausea, and sleepiness. Patients with narrow-angle glaucoma or patients with liver or kidney diseases should not take duloxetine. Because duloxetine can cause liver damage, patients who drink large quantities of alcoholic beverages should not take it.
Tricyclic Antidepressants. Tricyclics are an older type of antidepressant. Tricyclics used for treatment of anxiety disorder include imipramine (Tofranil and generic, for generalized anxiety disorder, panic disorder), nortriptyline (Pamelor and generic, for panic disorder), desipramine (Norpramin and generic, for panic disorder), and clomipramine (Anafranil and generic, for obsessive compulsive disorder). Clomipramine is approved specifically for OCD, but because of its severe side effects it is usually used only if SSRIs have failed to help.
Side effects of tricyclic antidepressants (TCAs) include sleep disturbance, abrupt reduction in blood pressure upon standing, weight gain, sexual dysfunction, and mental disturbance. Elderly patients and those with a history of seizures, cardiac problems, closed-angle glaucoma, and urinary retention or obstruction should be closely supervised when taking tricyclics.
[For more information on antidepressant medications, see In-Depth Report #08: Depression.]
Benzodiazepines
Benzodiazepines are effective medications for most anxiety disorders and have been the standard of treatment for years. However, their longterm daily use is associated with a risk for dependency and abuse. Therefore, they have been replaced in most cases by SSRIs and other newer antidepressants.
For anxiety disorders, benzodiazepines are most often used to treat panic disorder, and are sometimes used for social anxiety disorder and generalized anxiety disorder. These drugs include alprazolam (Xanax, generic), clonazepam (Klonopin, generic), and lorazepam (Ativan, generic).
Benzodiazepines can have many side effects, which are generally associated with chronic use. The most common are daytime drowsiness and a hung-over feeling. In rare cases, they can cause agitation. They may worsen respiratory problems. Benzodiazepines are potentially dangerous when used in combination with alcohol. Overdoses can be serious, although they are very rarely fatal.
Older people are more susceptible to side effects and should usually start at half the dose prescribed for younger people. These drugs increase the risk of falling, which can increase the risk for hip fracture in older people. Also of concern are studies showing a high risk of automobile accidents in people who take benzodiazepines. Benzodiazepines taken during pregnancy are associated with birth defects (such as cleft palate), and they should not be used by pregnant women or by nursing mothers.
Loss of Effectiveness and Dependence. Eventually these drugs can lose their effectiveness with continued use at the same dosage. As a result, patients may want to increase their dosage to prevent anxiety. This causes dependency, which can occur after taking these drugs for several weeks.
Withdrawal and its Treatments. Withdrawal symptoms can be very severe, even in people who rapidly discontinue benzodiazepines after taking them for only 4 weeks. Symptoms include sleep disturbance and anxiety, which can develop within hours or days after stopping the medication. Some patients experience stomach distress, sweating, and insomnia, which can last 1 - 3 weeks. The longer the drugs are taken and the higher their dose, the more severe these symptoms can become. Tapering off gradually is the best approach to stop taking these drugs. Certain medications (such as anti-seizure drugs, antidepressants, and buspirone) may also help with withdrawal.
Azapirones (Buspirone)
Azapirones, such as buspirone (BuSpar, generic), act on serotonin receptors called 5-HT(1A). Buspirone appears to work as well as a benzodiazepine for treating generalized anxiety disorder. It usually takes several days to weeks for the drug to be fully effective. It is not useful against panic attacks.
Buspirone does not produce any immediate euphoria or change in sensation, so some people believe, erroneously, that the drug doesn't work. Such qualities result in a very low potential for abuse. Unlike the benzodiazepines, buspirone is not addictive, even with long-term use, so it may be particularly helpful for the patient whose anxiety disorder coexists with alcoholism or drug abuse.
Buspirone tends to have less pronounced side effects than benzodiazepines and no withdrawal effects, even when the drug is discontinued quickly. Common side effects include dizziness, drowsiness, and nausea. Buspirone should not be used with monoamine oxidase inhibitors (MAOIs).
Beta Blockers
Beta blockers, including propranolol (Inderal, generic) and atenolol (Tenormin, generic), block the nerves that stimulate the heart to beat faster. They affect only the physiologic symptoms of anxiety (particularly rapid heart rate) and are most helpful for phobias, particularly performance anxiety. They may be taken before entering a situation where anxiety symptoms tend to occur. Beta blockers are less effective for other forms of anxiety.
Atypical Antipsychotics
Atypical antipsychotics are mostly used for treating schizophrenia, bipolar disorder, and major depressive disorder. They may sometimes be used for treating severe cases of OCD or PTSD. However, atypical antipsychotics (particularly olanzapine) can have severe side effects. These include weight gain and increased high blood sugar levels, which can increase the risk for diabetes. [For more information, see In-Depth Report #47: Schizophrenia.]
Anticonvulsants (Antiseizure Drugs)
Pregabalin (Lyrica) and gabapentin (Neurontin, generic) are drugs used to treat seizures and other conditions. Researchers are investigating whether these drugs may be useful for certain anxiety disorders, such as social anxiety disorder and general anxiety disorder. Their exact role in the treatment of anxiety disorders is not clear, however.
Psychotherapy and Other Treatments
Cognitive-Behavioral Therapy
The goal of cognitive-behavioral therapy (CBT) is to regain control of reactions to stress and stimuli, thus reducing the feeling of helplessness that often accompanies anxiety disorders. CBT works on the principle that the thoughts that produce and maintain anxiety can be recognized and altered using various techniques that change behavioral responses and eliminate the anxiety reaction.
CBT and medication are each effective alone but many studies have shown that a combination of CBT and medication works best for treating anxiety disorders. Combination CBT and medication is particularly effective for children and adolescents. Evidence clearly supports the combination approach’s benefits for treating pediatric cases of generalized anxiety disorder, separation anxiety, social phobia, and obsessive compulsive disorder.
Studies suggest that CBT is also helpful for patients who have additional conditions, such as depression, a second anxiety disorder, or alcohol dependency. (It may take longer to achieve a successful outcome in such cases, however.)
Both individual and group treatments work well. However, people with social phobia may do better in individual sessions.
Anxiety disorders are chronic and recurrence is common, even after successful short-term therapy. Some patients with anxiety disorders may require long-term or intensive therapy of at least a year or 50 sessions. Medications, then, are also generally recommended for most patients.
Basic Cognitive Therapy Techniques. Treatment usually takes about 12 - 20 weeks. The essential goal of cognitive therapy is to understand the realities of an anxiety-provoking situation and to respond to reality with new actions based on reasonable expectations.
- First, the patient must learn how to recognize anxious reactions and thoughts as they occur. One way of accomplishing this is by keeping a daily diary that reports the occurrences of anxiety attacks and any thoughts and events associated with them. A patient with OCD, for instance, may record repetitive thoughts.
- These entrenched and automatic reactions and thoughts must be challenged and understood. Using the OCD example, one approach is to record and play back the words of the repetitive thoughts, overexposing the patient to the thoughts and reducing their effect. For patients with generalized anxiety disorder, CBT targets their intolerance of uncertainty and helps them develop methods to cope with it.
- Patients are usually given behavioral homework assignments to help them change their reactions. For example, a person with generalized social phobia may be asked to buy an item and then return it the next day. As patients perform these actions, they learn to recognize fears and thoughts triggered by similar events and to understand that these fears are unrealistic.
- As the patient continues with self-observation, they begin to perceive the false assumptions that underlie the anxiety. For example, patients with OCD may learn to recognize that their heightened sense of responsibility for preventing harm in non-threatening situations is neither necessary nor useful.
- At that point, the patient can begin substituting new ways of coping with the feared objects and situations.
Systematic Desensitization. Systematic desensitization is a specific technique that breaks the link between the anxiety-provoking stimulus and the anxiety response. This treatment requires the patient to gradually confront the object of fear. There are three main elements to the process:
- Relaxation training
- A list composed by the patient that prioritizes anxiety-inducing situations by degree of fear
- The desensitization procedure itself, confronting each item on the list, starting with the least stressful
This treatment is especially effective for simple phobias, social phobias, agoraphobia, and post-traumatic stress syndrome.
Exposure and Response Treatment. Exposure treatment purposefully generates anxiety by exposing the patient repeatedly to the feared object or situation, either literally or using imagination and visualization. It uses the most fearful stimulus first. (This differs from the desensitization process because it does not involve relaxation or a gradual approach to the source of anxiety.)
Exposure treatments are usually known as either flooding or graduated exposure:
- Flooding exposes the person to the anxiety-producing stimulus for as long as 1 - 2 hours.
- Graduated exposure gives the patient a greater degree of control over the length and frequency of exposures.
In both cases, the patient experiences the anxiety over and over until the stimulating event eventually loses its effect. Combining exposure with standard cognitive therapy may be particularly beneficial. This approach has helped certain patients in most anxiety disorder categories, including post-traumatic stress disorder.
Modeling Treatment. Phobias can often be treated successfully with modeling treatment:
- The therapy typically uses an actor who approaches an anxiety-producing object or engages in a fear-provoking activity that is similar to the patient's specific problem. Either a live or videotaped situation may be used, although the live model is considered to be more effective.
- The patient observes this event and tries to learn how to behave in a comparable manner.
Other Forms of Psychotherapy
Other forms of psychotherapy -- commonly called emotion-based psychotherapy (EBT), psychodynamic therapy, or "talk" therapy -- deal more with the roots of anxiety and usually, although not always, require longer treatments. They include interpersonal therapy, supportive psychotherapy, attention intervention, and psychoanalysis. All work is done during the sessions. Some research indicates that such therapies might be more useful for generalized anxiety, which may require more sustained work to process and recover from early traumas and fears. Studies suggest that although emotion-based psychotherapies are not as effective as cognitive-behavioral therapy (CBT) in treating panic disorders, patients tend to stay longer in EBT than in CBT. Some doctors recommend adding elements of EBT to the usual CBT and medication treatments.
Relaxation Training and Related Therapies
Relaxation Training. Relaxation techniques use muscle relaxation and mental visualization to help focus attention towards a calming feeling. Some people find meditation helpful.
Breathing Retraining. Breathing retraining techniques may help reduce the physical effects of anxiety. For example, hyperventilation is one of the primary physical manifestations of panic disorders. This involves rapid, tense breathing, resulting in chest pain, dizziness, tingling of the mouth and fingers, muscle cramps, and even fainting. By practicing measured, controlled breathing at the onset of a panic attack, patients may be able to prevent full attacks.
Biofeedback. Biofeedback uses special sensors that allow patients to recognize anxiety states by changes in specific physical functions, such as changes in pulse rate, skin temperatures, and muscle tone. Eventually they learn to modify these changes, which in turn helps relieve anxiety. While commonly used, there are not many rigorous studies showing that biofeedback helps patients reduce or eliminate their symptoms over the long term.
Psychological Therapies for Post-Traumatic Stress Disorder (PTSD)
Several types of psychological treatments have been designed specifically for treating patients with PTSD. These approaches include a special type of CBT known as trauma-focused cognitive behavioral therapy (TFCBT), and a psychotherapy treatment called eye movement desensitization and reprocessing (EMDR).
With TFCBT, patients are taught stress management skills. The therapist helps the patient develop a narrative (verbal, written, or artistic) about the traumatic event. Patients may be exposed to reminders about the trauma and are taught how to cope with future reminders. Through the process, the patient learns how to reprocess their thoughts, feelings, and behaviors.
With EMDR, the patient focuses on remembering the traumatic experience while visually following the rhythmic movement of the therapist’s fingers. The patient recounts to the therapist what memories have been provoked during the exercise. EMDR may help patients recall details and sensations that they had blocked out. Through this breakthrough, patients learn how to regain emotional control.
Herbs and Supplements
Generally, manufacturers of herbal remedies and dietary supplements do not need FDA approval to sell their products. Just like a drug, herbs and supplements can affect the body's chemistry, and therefore have the potential to produce side effects that may be harmful. There have been a number of reported cases of serious and even lethal side effects from herbal products. Always check with your doctor before using any herbal remedies or dietary supplements.
Some studies suggest that the dietary supplement inositol may have benefits for panic disorder and, possibly, obsessive compulsive disorder. Inositol is part of the vitamin B complex.
Some patients use aromatherapy as a relaxation aid. Aromatherapy is in general safe, but some plant extracts in these formulas have been linked to skin allergies.
There is no evidence supporting the efficacy of valerian, St. John's wort, or passionflower for treatment of anxiety. The herbal remedy kava has been associated with liver problems and should not be used. Kava can also interact dangerously with medications that are metabolized by the liver.
Deep Brain Stimulation (DBS)
Deep brain stimulation (DBS) is a surgical approach that involves implanting in the brain a small device similar to a pacemaker. In 2009, the FDA approved a deep brain stimulation device (Reclaim) for treatment of chronic, severe, and disabling obsessive compulsive disorder (OCD). This is the first medical device approved for treatment of OCD.
The device is similar to other DBS devices used for treating movement disorders like Parkinson’s disease. It uses four electrodes that are surgically implanted into the brain and connected by wires to a small generator that is implanted near the abdomen or collar bone. The generator delivers precisely controlled electrical pulses to target specific areas of the brain.
Another brain stimulation approach, transcranial magnetic stimulation (TMS), does not involve surgery or implantation. It uses an external machine to generate high frequency magnetic pulses to target and stimulate areas of the brain. TMS is also being studied as a possible treatment for OCD.
Surgery
A surgical technique called cingulotomy involves interrupting the cingulate gyrus, a bundle of nerve fibers in the front of the brain. It is sometimes used as a last resort for patients with severe OCD.
Resources
- www.nimh.nih.gov -- National Institute of Mental Health
- www.adaa.org -- Anxiety Disorders Association of America
- www.nami.org -- National Alliance on Mental Illness
- www.psych.org -- The American Psychiatric Association
- www.apa.org -- The American Psychological Association
- www.istss.org -- International Society for Traumatic Stress Studies
- www.ncptsd.va.gov -- National Center for Post-Traumatic Stress Disorders
- www.aacap.org -- American Academy of Child and Adolescent Psychiatry
- www.ocfoundation.org -- International OCD Foundation
References
ACOG Committee on Practice Bulletins--Obstetrics. ACOG Practice Bulletin: Clinical management guidelines for obstetrician-gynecologists number 92, April 2008 (replaces practice bulletin number 87, November 2007). Use of psychiatric medications during pregnancy and lactation. Obstet Gynecol. 2008 Apr;111(4):1001-20.
American Academy of Child and Adolescent Psychiatry. Practice parameter on the use of psychotropic medication in children and adolescents. J Am Acad Child Adolesc Psychiatry. 2009 Sep;48(9):961-73.
Baldwin D, Woods R, Lawson R, Taylor D. Efficacy of drug treatments for generalised anxiety disorder: systematic review and meta-analysis. BMJ. 2011 Mar 11;342:d1199. doi: 10.1136/bmj.d1199.
Bisson J, Andrew M. Psychological treatment of post-traumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2007 Jul 18;(3):CD003388.
Bisson JI. Post-traumatic stress disorder. BMJ. 2007 Apr 14;334(7597):789-93.
Bridge JA, Iyengar S, Salary CB, et al. Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: a meta-analysis of randomized controlled trials. JAMA. 2007 Apr 18;297(15):1683-96.
Burstein M, Ameli-Grillon L, Merikangas KR. Shyness versus social phobia in US youth. Pediatrics. 2011 Nov;128(5):917-25. Epub 2011 Oct 17.
Cohen JA, Bukstein O, Walter H, Benson SR, Chrisman A, Farchione TR, et al. Practice parameter for the assessment and treatment of children and adolescents with posttraumatic stress disorder. J Am Acad Child Adolesc Psychiatry. 2010 Apr;49(4):414-30.
Connolly SD, Bernstein GA; Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2007 Feb;46(2):267-83.
Fenske JN, Schwenk TL. Obsessive compulsive disorder: diagnosis and management. Am Fam Physician. 2009 Aug 1;80(3):239-45.
Gale C, Davidson O. Generalised anxiety disorder. BMJ. 2007 Mar 17;334(7593):579-81.
Ebell MH. Diagnosis of anxiety disorders in primary care. Am Fam Physician. 2008 Aug 15;78(4):501-2.
Gale C, Davidson O. Generalised anxiety disorder. BMJ. 2007 Mar 17;334(7593):579-81.
Heyman I, Mataix-Cols D, Fineberg NA. Obsessive-compulsive disorder. BMJ. 2006 Aug 26;333(7565):424-9.
Hofmann SG, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry. 2008 Apr;69(4):621-32.
Hunot V, Churchill R, Silva de Lima M, Teixeira V. Psychological therapies for generalised anxiety disorder. Cochrane Database Syst Rev. 2007 Jan 24;(1):CD001848.
Ipser JC, Stein DJ, Hawkridge S, Hoppe L. Pharmacotherapy for anxiety disorders in children and adolescents. Cochrane Database Syst Rev. 2009 Jul 8;(3):CD005170.
Katon WJ. Clinical practice. Panic disorder. N Engl J Med. 2006 Jun 1;354(22):2360-7.
Kodish I, Rockhill C, Ryan S, Varley C. Pharmacotherapy for anxiety disorders in children and adolescents. Pediatr Clin North Am. 2011 Feb;58(1):55-72, x.
Koran LM, Hanna GL, Hollander E, Nestadt G, Simpson HB; American Psychiatric Association. Practice guideline for the treatment of patients with obsessive-compulsive disorder. Am J Psychiatry. 2007 Jul;164(7 Suppl):5-53.
Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007 Mar 6;146(5):317-25.
Leichsenring F, Rabung S. Effectiveness of long-term psychodynamic psychotherapy: a meta-analysis. JAMA. 2008 Oct 1;300(13):1551-65.
Maher AR, Maglione M, Bagley S, Suttorp M, Hu JH, Ewing B, et al. Efficacy and comparative effectiveness of atypical antipsychotic medications for off-label uses in adults: a systematic review and meta-analysis. JAMA. 2011 Sep 28;306(12):1359-69.
North CS, Suris AM, Davis M, Smith RP. Toward validation of the diagnosis of posttraumatic stress disorder. Am J Psychiatry. 2009 Jan;166(1):34-41. Epub 2008 Dec 1.
Roberts NP, Kitchiner NJ, Kenardy J, Bisson JI. Systematic review and meta-analysis of multiple-session early interventions following traumatic events. Am J Psychiatry. 2009 Mar;166(3):293-301. Epub 2009 Feb 2.
Saeed SA, Bloch RM, Antonacci DJ. Herbal and dietary supplements for treatment of anxiety disorders. Am Fam Physician. 2007 Aug 15;76(4):549-56.
Schneier FR. Clinical practice. Social anxiety disorder. N Engl J Med. 2006 Sep 7;355(10):1029-36.
Smoller JW, Pollack MH, Wassertheil-Smoller S, et al. Panic attacks and risk of incident cardiovascular events among postmenopausal women in the Women's Health Initiative Observational Study. Arch Gen Psychiatry. 2007 Oct;64(10):1153-60.
Soomro GM, Altman D, Rajagopal S, Oakley-Browne M. Selective serotonin re-uptake inhibitors (SSRIs) versus placebo for obsessive compulsive disorder (OCD). Cochrane Database Syst Rev. 2008 Jan 23;(1):CD001765.
Stein MB, Goin MK, Pollack MH, Roy-Byrne P, Sareen J, Simon NM, et al. Practice guideline for the treatment of patients with panic disorder. Arlington, VA: American Psychiatric Association, 2009.
Stein MB, Stein DJ. Social anxiety disorder. Lancet. 2008 Mar 29;371(9618):1115-25.
Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, et al. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. N Engl J Med. 2008 Oct 31. [Epub ahead of print]
Watanabe N, Churchill R, Furukawa TA. Combined psychotherapy plus benzodiazepines for panic disorder. Cochrane Database Syst Rev. 2009 Jan 21;(1):CD005335.
|
Review Date:
2/8/2012 Reviewed By: Harvey Simon, MD, Editor-in-Chief, Associate Professor of Medicine, Harvard Medical School; Physician, Massachusetts General Hospital. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc. |


